Analgesic
An analgesic, known colloquially as a painkiller, is any natural or synthetic drug that relieves pain (produces analgesia) without causing loss of consciousness, paralysis, or other major impairment of sensory function or nerve impulse conduction. The word analgesic derives from Greek an- ("without") and -algia ("pain"). The term analgesia refers to an absence of the sensation of pain while still being conscious.
An analgesic is any member of a diverse group of drugs used to relieve pain. There are two basic categories of analgesics: Opioids or narcotic analgesics and nonopioids. Opioids comprise natural source drugs derived from opium, especially morphine and codeine, and semi-synthetic drugs like meperidine (Demerol, propoxyphen (Darvon)), and oxycodone (Uretsky 2002). Nonopioids include the non-steroidal anti-inflammatory drugs (NSAIDs) (such as aspirin and ibuprofen) and acetaminophen. Other drugs not normally classified as analgesics also have been used to relieve pain. These include tricyclic antidepressants and anti-epileptic agents such as gabapentin (Uretsky 2002).
Analgesic drugs act in various ways on the peripheral (PNS) and central nervous systems (CNS), either blocking the signal from the PNS or distorting the interpretation by the CNS (Uretsky 2002).
Medical researchers have developed widely diverse compounds for treating pain, including some synthetic opioids that produce an analgesic effect but that are much less likely to induce dependency. It is important to note that some pain is productive, acting as a warning of injury and a guide to diagnosis and treatment; thus it is also important to realize that while analgesics relieve symptoms, they do not affect the underlying cause (Uretsky 2002).
The major classes
The two major types of analgesics are opioids and nonopioids.
The type of analgesic used depends on the severity of pain—whether it is acute (self-limiting in duration, such as childbirth) or chronic (lasting more than three months)—and the response to other medications (Uretsky 2002). The World Health Organization's "pain ladder," originally developed for cancer-related pain, is a widely used protocol for determining in a stepwise manner the suitable drug and dosage for treating pain (WHO 1990). The choice of analgesia is also determined by the type of pain: for neuropathic pain, traditional analgesia is less effective, and there is often benefit from classes of drugs that are not normally considered analgesics, such as tricyclic antidepressants and anticonvulsants (Dworkin et al. 2003).
Opioid analgesics
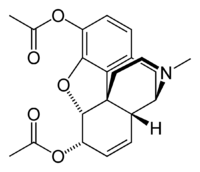
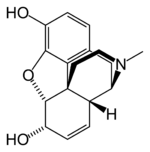
Opioid analgesics, known also as "narcotic analgesics," are analgesics derived from opium, as well as semi-synthetics and even synthetics that behave pharmacologically like morphine, and are pain relievers that act on the central nervous system (Uretsky 2002; Ross-Flanigan 2002). The archetypal opioid is morphine, a derivative of the opium poppy. The morphine molecule is the chemical basis of many painkillers, some with minimal abuse potential (Uretsky 2002). In addition to morphine, other narcotic analgesics include codeine, oxycodone, propoxyphene (Darvon), hydrocodone, and diacetylmorphine (heroin, meperidine (Demerol), and pethidine). All exert a similar influence on the cerebral opioid receptor system. Tramadol and buprenorphine are thought to be partial agonists of the opioid receptors.
Opium is a narcotic formed from the latex (i.e., sap) released by lacerating (or "scoring") the immature seed pods of opium poppies (Papaver somniferum). The opium latex contains up to 16 percent morphine, as well as codeine and non-narcotic alkaloids, such as papaverine and noscapine. Heroin (diacetylmorphine or diamorphine) is a semi-synthetic opioid synthesized from morphine. As with other opiates, heroin can act both as a painkiller and a recreational drug. Codeine is an alkaloid found in opium. While it can be extracted from opium, most codeine is synthesized from morphine through the process of O-methylation. Codeine is by far the most widely used opiate in the world and very likely most commonly used drug overall.
Opioids, while very effective analgesics, may have some unpleasant side-effects. Drowsiness, dizziness, and breathing problems are some unwanted side effects, as well as physical and mental dependence (Ross-Flanigan 2002). Like all narcotics, opioids can become habit-forming. In addition, up to one in three patients starting morphine may experience nausea and vomiting (generally relieved by a short course of antiemetics). Pruritus (itching) may require switching to a different opioid. Constipation occurs in almost all patients on opioids, and laxatives (lactulose, macrogol-containing or co-danthramer) are typically co-prescribed.
Dosing of all opioids may be limited by opioid toxicity (confusion, respiratory depression, myoclonic jerks and pinpoint pupils), but there is no dose ceiling in patients who tolerate this.
When used appropriately, opioid analgesics are otherwise safe and effective. However, risks such as addiction and the body becoming used to the drug are serious concerns. Due to the body getting used to the drug, often the dose must be increased. If the drug is being used for treating a chronic disease, the doctor may follow the pattern of the no ceiling limit. What must be remembered, however, is that although there is no upper limit there is a still a toxic dose even if the body has become used to lower doses. Frequent administration of heroin has a high potential for causing addiction and may quickly lead to tolerance. If a continual, sustained use of heroin for as little as three days is stopped abruptly, withdrawal symptoms can appear. This is much shorter than the withdrawal effects experienced from other common painkillers such as oxycodone and hydrocodone.
Nonopioids
The two main classes of nonopioids are the nonsteroidal anti-inflammatory drugs (NSAIDs), including the salicylates, and acetaminophen (paracetamol). NSAIDs also have antipyretic and anti-inflammatory effects—they reduce fever and inflammation. Acetaminophen is a non-narcotic analgesic that lacks anti-inflammatory effects.
Acetyaminophen
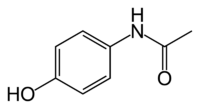
Acetaminophen (USAN) or paracetamol (International Nonproprietary Name) is a popular analgesic and antipyretic (fever-reducing) drug that is used for the relief of headaches, fever, and minor aches and pains, such as pain in joints and muscles. It is a major ingredient in numerous cold and flu medications and many prescription analgesics. When used responsibly in standard doses, it is considered effective and safe, but because of its wide availability and narrow therapeutic index, accidental or deliberate overdoses are not uncommon. Excessive doses lead to hepatotoxicity (liver damage).
Acetaminophen is an organic compound that inhibits synthesis of prostagladins in the central nervous system, thus raising the body's pain threshold, and further impacts the temperature-regulating center of the brain, thus reducing fever. Its exact mechanism is still poorly understood. Since it lacks anti-inflammatory properties, it is not a member of the class of drugs known as non-steroidal anti-inflammatory drugs. In normal doses, acetaminophen is less likely than NSAIDs to irritate the lining of the stomach and cause peptic ulcers, and does not affect blood coagulation, the kidneys, or the fetal ductus arteriosus (as NSAIDS can). It is a possible alternative for people allergic to NSAIDs or who are using anticoagulants.
NSAIDs
NSAIDs are analgesics with antipyretic and anti-inflammatory effects. The term "non-steroidal" is used to distinguish these drugs from steroids, which (among a broad range of other effects) have a similar eicosanoid-depressing, anti-inflammatory action. The most prominent members of this group of drugs are aspirin, ibuprofen, and naproxen partly because they are available over-the-counter in many areas.
Aspirin and the other NSAIDs inhibit cyclooxygenase, leading to a decrease in prostaglandin production; this reduces pain and also inflammation (in contrast to acetaminophen and the opioids).
Beginning in 1829, with the isolation of salicin from the folk remedy willow bark, NSAIDs have become an important part of the pharmaceutical treatment of pain (at low doses) and inflammation (at higher doses). Part of the popularity of NSAIDs is that, unlike opioids, they do not produce sedation or respiratory depression and have a very low addiction rate. NSAIDs, however, are not without their own problems. NSAIDs predispose to peptic ulcers, renal failure, and allergic reactions.
Certain NSAIDs, including ibuprofen and aspirin, have become accepted as relatively safe and are available over-the-counter without prescription. The use of certain NSAIDs in children under 16 suffering from viral illness may contribute to Reye's syndrome.
COX-2 inhibitors
These drugs have been derived from NSAIDs. The cyclooxygenase enzyme inhibited by NSAIDs was discovered to have at least two different versions: COX1 and COX2. Research suggested that most of the adverse effects of NSAIDs were mediated by blocking the COX1 (constitutive) enzyme, with the analgesic effects being mediated by the COX2 (inducible) enzyme. The COX2 inhibitors were thus developed to inhibit only the COX2 enzyme (traditional NSAIDs block both versions in general). These drugs (such as rofecoxib and celecoxib) are equally effective analgesics when compared with NSAIDs, but cause less gastrointestinal hemorrhage in particular. However, post-launch data indicated increased risk of cardiac and cerebrovascular events with these drugs due to an increased likelihood of clotting in the blood due to a decrease in the production of protoglandin around the platelets causing less clotting factor to be released, and rofecoxib was subsequently withdrawn from the market. The role for this class of drug is hotly debated. Illnesses inadvertently caused by doctors and medical treatments, called Iatrogenic diseases, are possible when the treatment affects the patient's blood, respiration, digestive processes and other bodily functions and organs.
Other agents
In patients with chronic or neuropathic pain, various other substances may have analgesic properties, but are not typically classified as analgesics. Tricyclic antidepressants, especially amitriptyline, have been shown to improve pain in what appears to be a central manner. The exact mechanism of carbamazepine, gabapentin, and pregabalin is similarly unclear, but these anticonvulsants are used to treat neuropathic pain with modest success.
Specific forms and uses
Combinations
Analgesics are frequently used in combination, such as the acetaminophen and codeine preparations found in many non-prescription pain relievers. Propoxyphene and acetaminophen are used together (Darvocet N), as are oxydodone and acetaminophen (Percocet, Roxicet), and hydrocodone and acetaminophen (Lortab, Anexsia) (Ross-Flanigan 2002). Analgesics also can be found in combination with vasoconstrictor drugs such as pseudoephedrine for sinus-related preparations, or with antihistamine drugs for allergy sufferers.
The use of acetaminophen (paracetamol), as well as aspirin, ibuprofen, naproxen, and other NSAIDs concurrently with weak to mid-range opiates (up to about the hydrocodone level) has been shown to have beneficial synergistic effects by combating pain at multiple sites of action—NSAIDs reduce inflammation that in some cases, is the cause of the pain itself while opiates dull the perception of pain. Thus, in cases of mild to moderate pain caused in part by inflammation, it is generally recommended that the two be prescribed together (Mehlisch 2002).
Topical or systemic
Topical analgesia is generally recommended to avoid systemic side-effects. Painful joints, for example, may be treated with an ibuprofen- or diclofenac-containing gel; capsaicin also is used topically. Lidocaine, an anesthetic, and steroids may be injected into painful joints for longer-term pain relief. Lidocaine is also used for painful mouth sores and to numb areas for dental work and minor medical procedures.
Psychotropic agents
Tetrahydrocannabinol (THC) and some other cannabinoids, either from the Cannabis sativa plant or synthetic, have analgesic properties, although the use of cannabis derivatives is illegal in many countries. Other psychotropic analgesic agents include ketamine (an NMDA receptor antagonist), clonidine and other α2-adrenoreceptor agonists, and mexiletine and other local anaesthetic analogues.
Atypical and/or adjuvant analgesics
Orphenadrine, cyclobenzaprine, scopolamine, atropine, gabapentin, first-generation antidepressants, and other drugs possessing anticholinergic and/or antispasmodic properties are used in many cases along with analgesics to potentiate centrally acting analgesics such as opioids when used against pain especially of neuropathic origin and to modulate the effects of many other types of analgesics by action in the parasympathetic nervous system. Dextromethorphan has been noted to slow the development of tolerance to opioids and exert additional analgesia by acting upon the NMDA receptors; some analgesics such as methadone and ketobemidone and perhaps piritramide have intrinsic NMDA action.
The use of adjuvant analgesics is an important and growing part of the pain-control field and new discoveries are made practically every year. Many of these drugs combat the side effects of opioid analgesics—an added bonus. For example, antihistamines, including orphenadrine, combat the release of histamine caused by many opioids, methylphenidate, caffeine, ephedrine, dextroamphetamine, and cocaine and work against heavy sedation and may elevate mood in distressed patients as do the antidepressants.
Addiction
Morphine and related compounds derived from opium—opiates—have the common attribute of having strongly additive properties. Withdrawal effects occur if the drug is stopped, including such symptoms as severe pain, sweating, confusion, and restlessness. While they have strong analgesic effects, with morphine being the most powerful medical analgesic, they also are strongly addictive.
Drugs have been synthesized to have similar structure as morphine, but less addictive. Semi-synthetics include meperideine (Demerol) and propoxyphen (Darvon). Some, such as methadone and meperidine have strong analgesic properties and are less (but still) addictive. Some semi-synthetics are even less addictive but considerably less strong in their analgesic properties (oxycodone, propoxyhene, etc.).
In the United States in recent years, there has been a wave of new addictions to prescription narcotics such as oxycodone and hydrocodone when available in pure formulations as opposed to combined with other medications (as in Percocet, which contains both oxycodone and acetaminophen/paracetamol, and Lortab, which contains hydrocodone and acetaminophen).
ReferencesISBN links support NWE through referral fees
- Dworkin, R. H, M. Backonja, M. C. Rowbotham, et al. 2003. Advances in neuropathic pain: Diagnosis, mechanisms, and treatment recommendations Arch. Neurol. 60(11): 1524-34. Retrieved April 29, 2008.
- Mehlisch, D. R. 2002. The efficacy of combination analgesic therapy in relieving dental pain J Am Dent Assoc 133(7): 861-71. Retrieved April 29, 2008.
- Ross-Flanigan, N. 2002. Analgesics, opioid. Pages 175-178 in J. L. Longe (ed.), The Gale Encyclopedia of Medicine, 2nd edition. Detroit, MI: Gale Group/Thomson Learning. ISBN 0787654892.
- Uretsky, S. 2002. Analgesics. Pages 173-175 in J. L. Longe (ed.), The Gale Encyclopedia of Medicine, 2nd edition. Detroit, MI: Gale Group/Thomson Learning. ISBN 0787654892.
- World Health Organization (WHO). 1990. Cancer pain relief and palliative care: Report of a WHO expert committee. Pages 1 to 75 in World Health Organization Technical Report Series, 804. Geneva Switzerland: World Health Organization. ISBN 924120804X.
| Analgesics (N02A, N02B) edit | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
N02BB Pyrazolones (Phenazone | Metamizole | Aminophenazone) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.